1 | Introduction
On April 21, 2021, the Government of Ontario (the Province) tabled in the Legislative Assembly volume 1 of the 2021-22 Expenditure Estimates.[1] The 2021-22 Expenditure Estimates (or Estimates) sets out the fiscal year’s spending requirements for ministries and constitutes the government’s formal request to the legislature for approval to spend the amounts as detailed in the Estimates.
After tabling in the legislature, the Estimates were referred to the Standing Committee on Estimates (SCE). The SCE is mandated to consider the Estimates of between six and 12 ministries. For 2021-22, the SCE has selected the Estimates of the following ministries for review:
- Health
- Natural Resources and Forestry
- Long-Term Care
- Education
- Infrastructure
- Agriculture, Food and Rural Affairs
- Children, Community and Social Services
- Energy, Northern Development and Mines
- Indigenous Affairs
After the SCE completes its review of a ministry, the committee votes on the ministry’s Estimates. Once the review and voting process is completed for all selected ministries, the SCE must deliver a report to the legislature by the third Thursday in November.[2] The legislature then votes its agreement of the Estimates passed by the SCE, after which the Supply Bill is formally introduced. Passage of the Supply Bill provides the legislature’s approval to spend the amounts as detailed in the Estimates.
The purpose of this report is to support the SCE’s review of the Ministry of Long-Term Care’s (MLTC’s) 2021-22 Expenditure Estimates. The report begins with a financial overview of the ministry, focusing on spending by Estimates categories and by program. Next, the report identifies key financial issues for the ministry. For this year, the FAO:
- forecasts ministry spending through 2029-30, based on ministry programs and commitments;
- reviews the Province’s long-term care bed expansion and redevelopment plans;
- projects the number of long-term care beds through 2029-30 and identifies risks to the supply of beds; and
- examines the Province’s commitment to increase daily direct care for long-term care residents.
Lastly, the report reviews proposed 2021-22 spending by program and identifies spending trends and program changes.
2 | Ministry Overview
The Ministry of Long-Term Care (MLTC) is projected to spend $6.9 billion in the 2021-22 fiscal year. This is an increase of $0.5 billion (8.4 per cent) from 2020-21 interim results reported in the 2021 Ontario Budget.[3]
Figure 2‑1 Projected Ministry of Long-Term Care spending in 2020-21 and 2021-22, $ billions
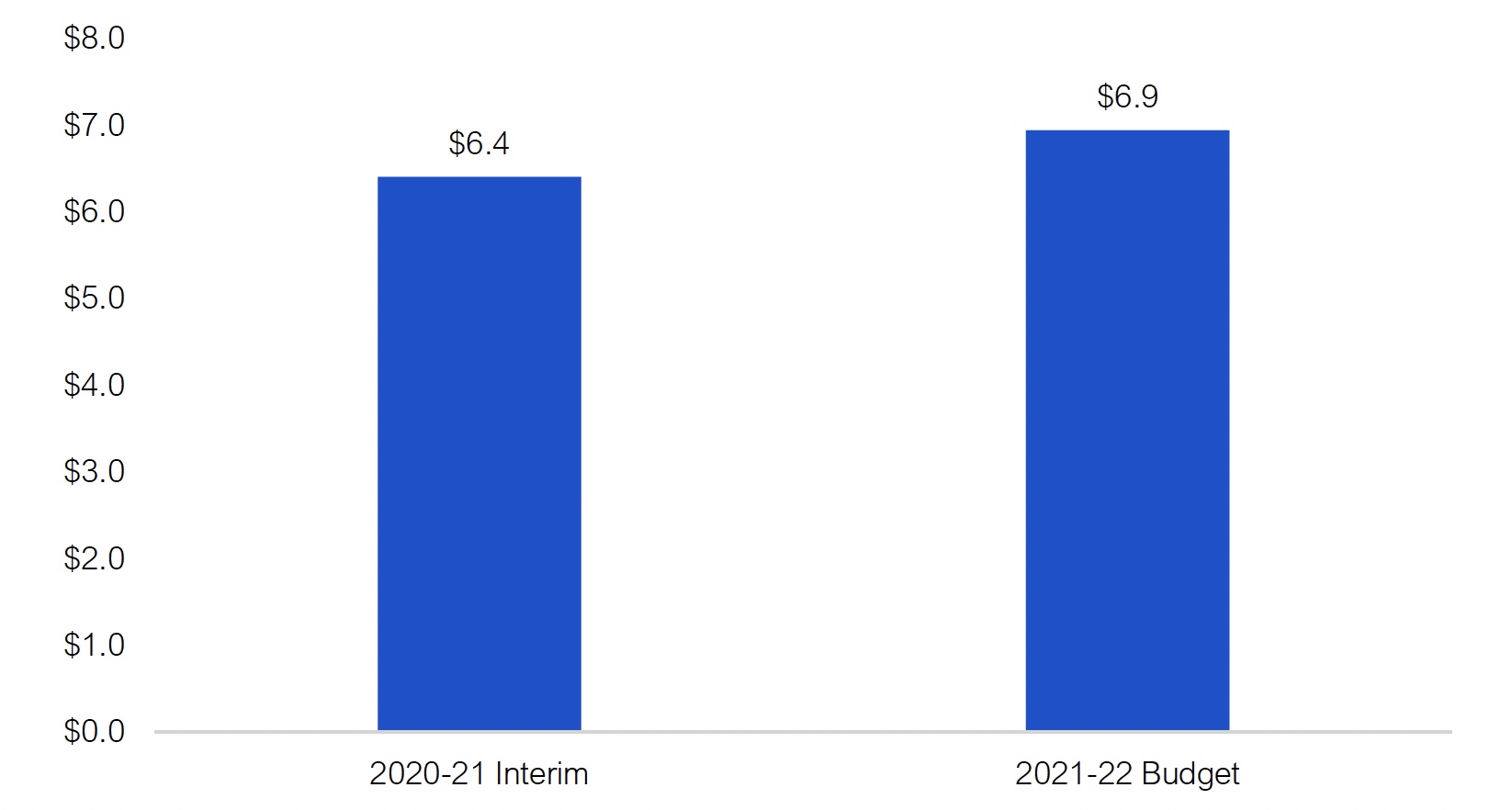
Note: Excludes negative adjustments of $4.5 billion in 2020-21 and $6.1 billion in 2021-22 to record expenses on the financial statements of Ontario Health and with the hospitals sector. These negative adjustments are offset by corresponding positive adjustments with the Ministry of Health.
Source: 2021-22 Expenditure Estimates, 2021 Ontario Budget and FAO analysis of information provided by the Ministry of Long-Term Care.
Accessible version
| Ministry of Long-Term Care Spending ($ billions) |
|
|---|---|
| 2020-21 Interim | 6.4 |
| 2021-22 Budget | 6.9 |
Spending by Expenditure Estimates Categories
The Ministry of Long-Term Care’s 2021-22 spending plan of $6.9 billion is reported as a net expense of $789 million in the 2021-22 Expenditure Estimates as follows:
- $6.9 billion in ‘Supply Bill spending’ that is authorized annually by the legislature (known as spending ‘to be voted’);
- Negative ‘other spending’ adjustments of $6.1 billion, to reverse planned payments by MLTC to long-term care (LTC) home operators and hospitals that will be recorded as expenses on the financial statements of Ontario Health and with the hospitals sector;[4] and
- Less than $1 million in spending that is authorized by standalone legislation (known as ‘statutory spending’).
Supply Bill spending is divided into programs called votes, sub-programs called items, and then accounts. The Ministry of Long-Term Care has two votes, with the Long-Term Care Homes Program accounting for almost all ministry spending at $6.9 billion.
Other spending includes a $5.6 billion negative adjustment for Ontario Health. This adjustment represents planned payments from the Ministry of Long-Term Care to LTC home operators that will be recorded as an expense on the financial statements of Ontario Health. There are also negative adjustments for hospitals of $48 million (operating) and $525 million (capital), which represent planned payments by the ministry that will be recorded as expenses in the hospitals sector.[5] Corresponding positive adjustments are included as ‘other spending’ in the Ministry of Health’s Expenditure Estimates.
Standalone legislation (i.e., spending authorized by legislation other than the Supply Bill) accounts for less than $1 million of planned MLTC spending.
| Vote | Program Name | 2021-22 Estimates ($ millions) |
|---|---|---|
| 4501 | Ministry Administration Program | 6 |
| 4502 | Long-Term Care Homes Program | 6,928 |
| Total Supply Bill (Voted) Spending | 6,934 | |
| Other spending – Ontario Health | -5,574 | |
| Other spending – hospitals (operating) | -48 | |
| Other spending – hospitals (capital) | -525 | |
| Total Other Spending Adjustments | -6,146 | |
| Standalone Legislation (Statutory) Spending | < 1 | |
| Net Ministry of Long-Term Care Expense | 789 |
For additional information on planned spending by Estimates categories, see chapter 4.
Spending by Program
Although the ministry is requesting authorization through the 2021-22 Expenditure Estimates to spend $6.9 billion, there is little information on how the ministry intends to spend the requested funds. The following presents the FAO’s overview of the ministry’s spending plan by program.
$6.3 billion of planned ministry spending in 2021-22 is from the net cost of two transfer payments to LTC home operators. There are 626 LTC homes in Ontario that have spaces for over 78,000 residents. LTC home operators receive funding from the ministry based on the number of beds each LTC home has in operation and the types of services the LTC home provides. In 2021-22, the FAO estimates that the operation of long-term care homes will cost a total of $7.9 billion, of which $1.6 billion will be recovered through resident co-payment revenue[6] and $6.3 billion will be funded by MLTC through two transfer payments, Long-Term Care Homes – Operations and Long-Term Care Homes – Development.
Of the $7.9 billion cost of long-term care home operations, an estimated $5.8 billion will be funded through a daily subsidy called the Level of Care (LOC) per diem payment. The LOC per diem is paid to LTC home operators for each bed in operation to cover the cost of nursing and personal care, basic accommodation, programs and support services, and raw food. Additionally, LTC home operators receive a global per diem that can be applied to any of the other four LOC categories.[7] The remaining $2.1 billion flows through a number of supplementary funding streams that includes one-time spending related to the COVID-19 pandemic.
The ministry also plans to spend $525 million in 2021-22 for capital projects, most of which is for the Accelerated Build Pilot Program. This program was developed in partnership with Infrastructure Ontario and three participating hospitals to accelerate the construction of four long-term care homes in the Greater Toronto Area. The funding for this program will be provided through the ministry’s third transfer payment program, Long-Term Care Homes Capital.
Finally, the ministry plans to spend $65 million on administration in 2021-22.
| Category | $ millions | |
|---|---|---|
| Level of Care Per Diem | ||
| Nursing and Personal Care | 3,290 | |
| Program and Support Services | 402 | |
| Raw Food | 285 | |
| Basic Accommodation | 1,674 | |
| Global Per Diem | 150 | |
| Total Level of Care Per Diem | 5,801 | |
| Supplementary Funding | ||
| Construction Funding Subsidy | 181 | |
| Pay Equity | 75 | |
| Municipal Tax Allowance Fund | 63 | |
| Behavioural Supports Ontario | 63 | |
| High Intensity Needs Fund | 77 | |
| Equalization Adjustment | 52 | |
| Resident Assessment Instrument | 42 | |
| Other Supplementary Funding | 749 | |
| One-Time COVID-19 Response Spending | 822 | |
| Total Supplementary Funding | 2,124 | |
| Total Cost of Long-Term Care Home Operations | 7,925 | |
| Less: Resident Co-payments | -1,580 | |
| Net Transfer Payments to Long-Term Care Home Operators* | 6,345 | |
| Ministry Administration | 65 | |
| Total Operating Spending | 6,410 | |
| Accelerated Build Pilot Program and other capital spending** | 525 | |
| Total Operating and Capital Spending | 6,935 |
3 | Key Issues for 2021-22
Spending Plan Analysis
This section provides a projection of Ministry of Long-Term Care spending through 2029-30. Note that in this section the FAO analyzes projected spending for the ministry before negative adjustments to record expenses on the financial statements of Ontario Health and the hospitals sector.[8]
The FAO reviewed the ministry’s programs and commitments and projects that long-term care spending will grow from $4.4 billion in 2019-20 to $10.6 billion by 2029-30. This represents an average annual growth rate over the 10-year period of 9.3 per cent.
Over the medium term, from 2019-20 to 2023-24, the FAO projects that ministry spending will grow at an average annual rate of 13.7 per cent, increasing from $4.4 billion in 2019-20 to $7.3 billion in 2023-24. The FAO’s projection is lower than the ministry’s spending plan in the 2021 Ontario Budget. The reason for the difference is that the FAO expects that new long-term care beds will come into service at a later date than reflected in the 2021 budget spending plan, resulting in the FAO’s lower spending forecast through 2023-24.
Over the long term, from 2023-24 through 2029-30, the FAO projects average annual spending growth of 6.4 per cent, reaching $10.6 billion by 2029-30. The FAO is not able to compare its spending forecast against the ministry’s over this period as the ministry reported to the FAO that, starting in 2024-25, the health sector spending plan in the 2021 budget is not allocated by program. In the 2021 budget, total health sector spending is projected to grow from $72.0 billion in 2023-24 to $82.0 billion in 2029-30. The FAO estimates that in order to fully fund long-term care programs and commitments, MLTC spending would require 33 per cent of new health sector spending in the 2021 budget plan over this period. This means that, after accounting for long-term care spending, the 2021 budget calls for the other health sector programs to grow by an average annual rate of only 1.6 per cent from 2023-24 to 2029-30.
Figure 3‑1 FAO projection for Ministry of Long-Term Care spending, 2019-20 to 2029-30, $ billions
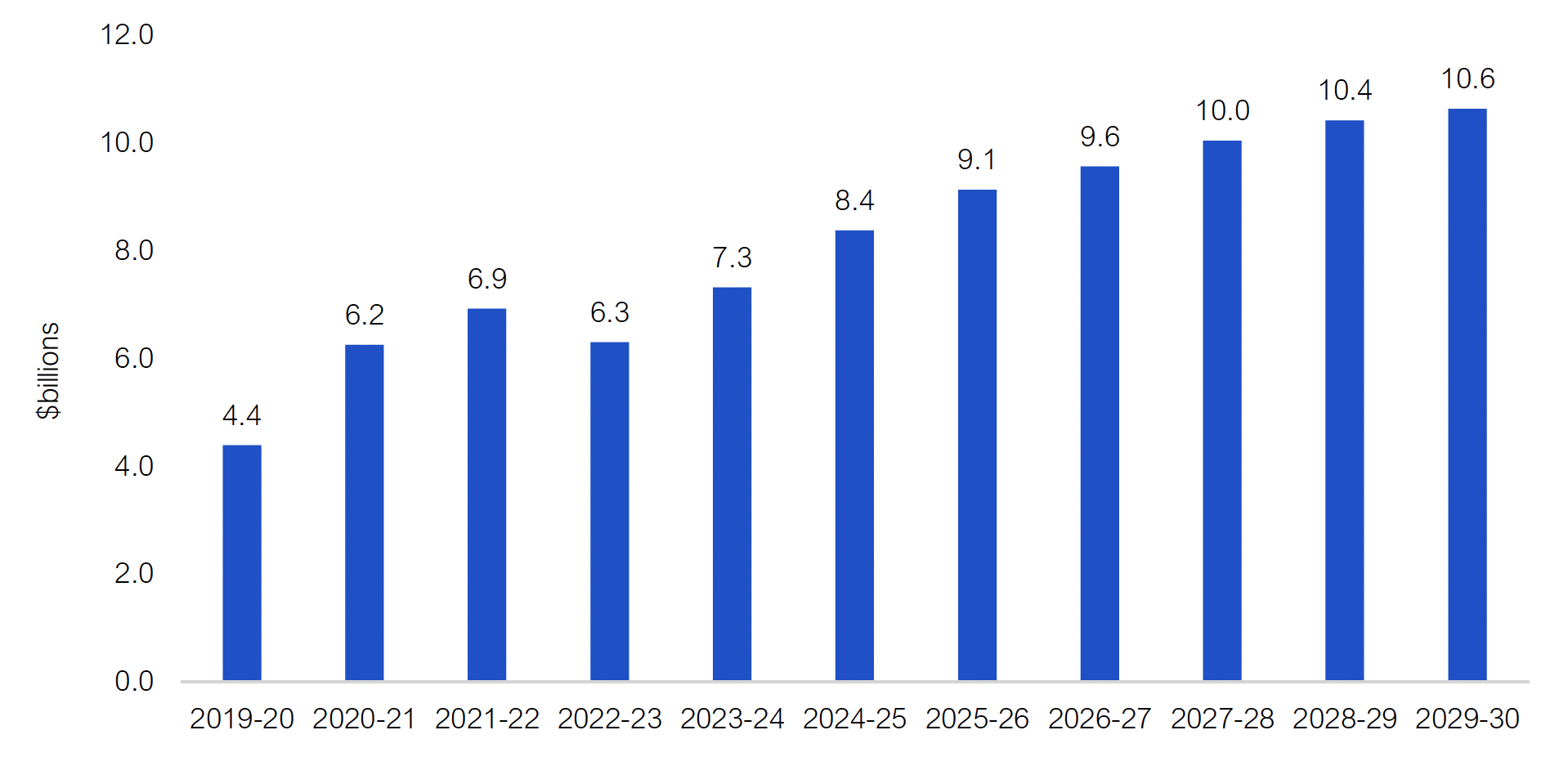
Source: FAO calculations.
Accessible version
| Fiscal Year | Ministry of Long-Term Care Spending ($ billions) |
|---|---|
| 2019-20 | 4.4 |
| 2020-21 | 6.2 |
| 2021-22 | 6.9 |
| 2022-23 | 6.3 |
| 2023-24 | 7.3 |
| 2024-25 | 8.4 |
| 2025-26 | 9.1 |
| 2026-27 | 9.6 |
| 2027-28 | 10.0 |
| 2028-29 | 10.4 |
| 2029-30 | 10.6 |
The FAO’s projected Ministry of Long-Term Care average annual spending growth from 2019-20 to 2029-30 of 9.3 per cent represents a significant increase compared to the previous 10-year period. From 2009-10 to 2019-20, long-term care spending grew at an average annual rate of only 3.0 per cent, increasing from $3.2 billion in 2009-10 to $4.4 billion in 2019-20.
The relatively high projected spending growth from 2019-20 to 2029-30 is primarily due to two significant long-term care commitments made by the Province:
- To expand and redevelop long-term care beds by:
- Building 30,000 new and redeveloped long-term care beds over 10 years.[9]
- Introducing a new long-term care development policy that increases provincial construction funding subsidies for new and redeveloped long-term care beds.
- To increase the average hours of daily direct care provided to long-term care residents by nurses and personal support workers from 2.75 hours per day in 2018 to four hours per day by 2024-25.[10]
The chart below shows how the Province’s two long-term care commitments affect the FAO’s spending projection. By 2023-24, the FAO estimates these two commitments will increase program spending by a total of $2.2 billion, which consists of $0.8 billion to expand and redevelop long-term care beds and $1.5 billion for the increase in daily direct care hours. By 2029-30, these commitments will increase program spending by $5.0 billion, which consists of $2.6 billion to expand and redevelop long-term care beds and $2.4 billion to increase daily direct care hours.
Finally, the FAO’s forecast incorporates a total of $3.2 billion in time-limited spending in 2020-21 and 2021-22. This includes approximately $2.5 billion in spending related to the COVID-19 pandemic for wage enhancements (pandemic pay) and operating costs (supplies, prevention and containment measures, and testing), and $0.7 billion for capital projects, most of which is for the Accelerated Build Pilot Program.
Figure 3‑2 Impact of provincial commitments and time-limited spending on projected Ministry of Long-Term Care spending, 2019-20 to 2029-30, $ billions
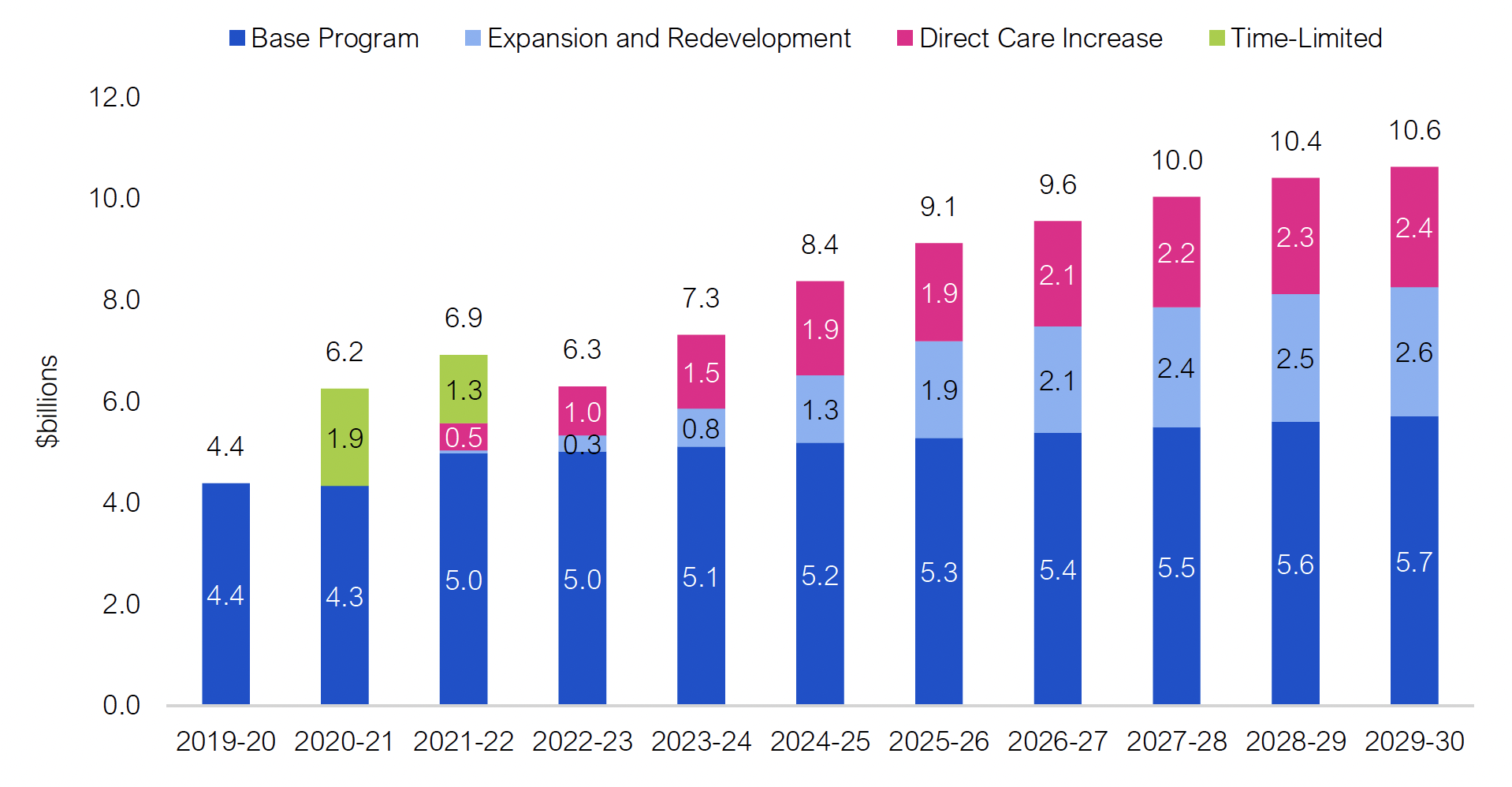
Source: FAO calculations.
Accessible version
| Fiscal Year | Base Program | Expansion and Redevelopment | Direct Care Increase | Time-Limited Spending | Total Spending |
|---|---|---|---|---|---|
| 2019-20 | 4.4 | 0.0 | 0.0 | 0.0 | 4.4 |
| 2020-21 | 4.3 | 0.0 | 0.0 | 1.9 | 6.2 |
| 2021-22 | 5.0 | 0.1 | 0.5 | 1.3 | 6.9 |
| 2022-23 | 5.0 | 0.3 | 1.0 | 0.0 | 6.3 |
| 2023-24 | 5.1 | 0.8 | 1.5 | 0.0 | 7.3 |
| 2024-25 | 5.2 | 1.3 | 1.9 | 0.0 | 8.4 |
| 2025-26 | 5.3 | 1.9 | 1.9 | 0.0 | 9.1 |
| 2026-27 | 5.4 | 2.1 | 2.1 | 0.0 | 9.6 |
| 2027-28 | 5.5 | 2.4 | 2.2 | 0.0 | 10.0 |
| 2028-29 | 5.6 | 2.5 | 2.3 | 0.0 | 10.4 |
| 2029-30 | 5.7 | 2.6 | 2.4 | 0.0 | 10.6 |
Expansion and Redevelopment Plan Analysis
The ministry’s long-term care bed expansion and redevelopment plan is part of the Province’s plan to address capacity issues in the health sector. As of December 2020, there were over 40,000 Ontarians on the wait list for a long-term care placement and the median wait time for a long-term care bed was 144 days. Long wait times for long-term care is a significant contributor to capacity issues in the health sector. The FAO estimates that patients waiting for a long-term care placement in hospitals occupied about five per cent of all hospital bed days in Ontario in 2017-18.[11]
The ministry’s plan also continues to address the 31,266 long-term care beds in Ontario that are not built to modern design standards. As noted by Ontario’s Long-Term Care COVID-19 Commission, these older beds make it “difficult, if not impossible, to manage the social distancing required during an infectious disease outbreak.”[12] Importantly, the Auditor General of Ontario found that almost two-thirds of the long-term care homes with the most severe outbreaks during the first wave of the COVID-19 pandemic had older bedroom designs.[13]
In this section, the FAO reviews the Province’s long-term care bed expansion and redevelopment plans. The Province has committed to build 30,000 new long-term care beds by 2028-29. In addition, although the Province has not committed to a long-term care bed redevelopment target,[14] the FAO assumes that the Province will redevelop at least 30,701 beds by 2028-29. Finally, to help facilitate the construction of new beds and the redevelopment of older beds, in July 2020, the Province introduced a new long-term care capital development policy that significantly increases provincial construction subsidies for eligible new and redeveloped long-term care beds.
The Commitment to Build 30,000 New Long-Term Care Beds
The Province’s commitment to build 30,000 new long-term care beds over 10 years from 2019-20 to 2028-29 builds on the previous commitment to build 15,000 new long-term care beds by 2023-24.[15] If achieved, 30,000 new long-term care beds by 2028-29 would represent a significant increase in the number of new beds compared to the prior 10-year period. From 2009-10 to 2018-19, the number of long-term care beds increased by 1,900.
The process to build a new long-term care bed begins when a long-term care operator signs a development agreement with the Ministry of Long-Term Care. Once the development agreement is executed, the LTC operator must finance and construct the beds in accordance with the terms of the agreement. Under normal circumstances, it takes approximately three years from the signing of a development agreement until a new long-term care bed opens.[16] However, due to the ongoing COVID-19 pandemic, the FAO estimates some timelines for existing projects will be delayed by up to 1.5 years.
As of March 2021, the Province has allocated 20,161 new long-term care beds.[17] The FAO projects most of these beds will come into service between 2023 and 2025. In order for the Province to achieve its goal of having all 30,000 new beds in service by the end of the 2028-29 fiscal year, the FAO estimates that the remaining bed allocations must be completed by March 2026.
The following chart outlines the FAO’s projection of when the 30,000 new beds will come into service. This projection incorporates actual project timelines for most of the 20,161 currently allocated beds and assumes that the Province will be successful in allocating the remaining 9,839 beds by March 2026 so that all 30,000 beds will be in service by 2028-29.
Figure 3‑3 FAO estimated cumulative in-service dates for 30,000 new long-term care beds
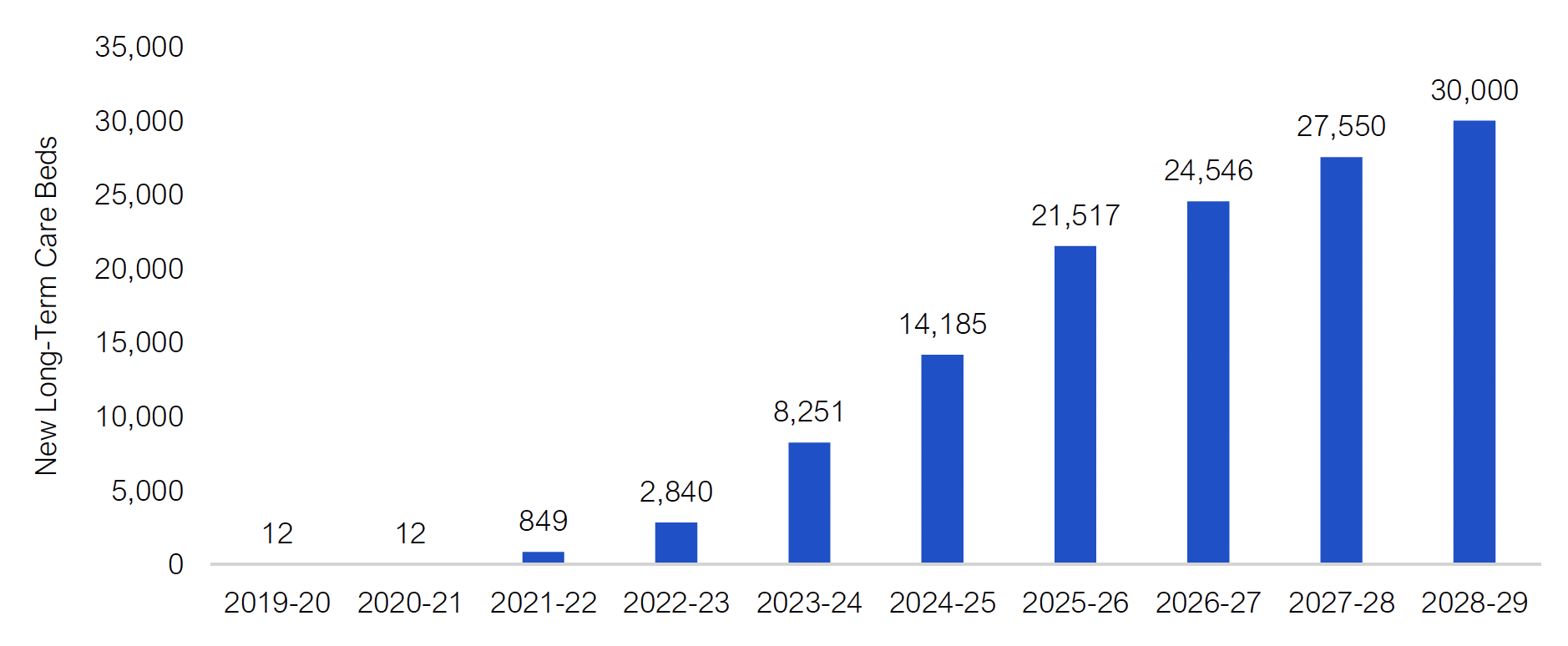
Source: FAO analysis of information provided by MLTC.
Accessible version
| Fiscal Year | New Long-Term Care Beds |
|---|---|
| 2019-20 | 12 |
| 2020-21 | 12 |
| 2021-22 | 849 |
| 2022-23 | 2,840 |
| 2023-24 | 8,251 |
| 2024-25 | 14,185 |
| 2025-26 | 21,517 |
| 2026-27 | 24,546 |
| 2027-28 | 27,550 |
| 2028-29 | 30,000 |
Importantly, the FAO estimates that only 8,251 new long-term care beds will be in service by the end of the 2023-24 fiscal year. This is well short of the Province’s previous commitment to add 15,000 new long-term care beds by 2023-24. Overall, the FAO projects that the Province will not reach 15,000 new long-term care beds until 2025-26.
The Plan to Redevelop Existing Long-Term Care Beds
The process for redeveloping long-term care beds is similar to building a new bed in that the LTC operator signs a development agreement with the Province. The LTC operator must then finance and construct the redeveloped beds in accordance with the terms of the agreement. Many LTC development projects currently underway in Ontario include both new and redeveloped beds.[18]
In Ontario, long-term care beds can have one of five structural classifications that depend on which design standards the beds meet. The following table outlines the structural classification of each of the Province’s 78,799 beds.
| Structural Classification | New | A | B | C | D | Unknown | Total |
|---|---|---|---|---|---|---|---|
| Number of Beds | 39,232 | 6,819 | 5,803 | 23,699 | 1,764 | 1,482 | 78,799 |
In total, there are 31,266 B, C and D class beds in Ontario that are not built to modern design standards. These beds were built to the design standards of the 1972 Nursing Homes Act Regulation, which allowed three and four beds per room and did not require washrooms in all resident bedrooms.[19] Redeveloped beds must comply with the Long-Term Care Home Design Manual 2015, which requires washrooms in all resident bedrooms and does not allow for more than two beds per room.[20]
Of the Province’s 31,266 B, C and D class beds, the licences for 26,531 of the Province’s B and C class beds will expire on June 30, 2025,[21] while the licences for the 1,764 D class beds expired in 2020. To be eligible for new licences, all of these beds will need to be redeveloped.[22] In addition, there are a total of 2,406 beds without expiring licences that are currently under redevelopment.[23] Consequently, the FAO estimates that the Province will need to redevelop at least 30,701 beds by 2028-29 to maintain the existing stock of long-term care beds.[24]
As of the writing of this report, the Province has allocated 15,918 beds for redevelopment, leaving an estimated 14,783 beds with expired (1,019 D class beds) or expiring (13,764 B and C class beds) licences that do not have redevelopment plans. The Province has publicly indicated that it intends to redevelop the 1,019 D class beds, while three years before the B and C class bed licences expire (June 2022), the Ministry of Long-Term Care must provide the operators of those LTC beds with notice of its intention to provide a new licence or not.[25] When the Long-Term Care Homes Act, 2007 was passed on July 1, 2010, B and C beds were provided with a transitional licence of 15 years.[26] To receive a new licence, these beds must comply with current design standards; therefore, the Ministry’s ability to grant a new licence will depend on the LTC operator’s willingness and ability to redevelop the beds. The ministry has indicated that it aims to reallocate any expiring beds that LTC operators chose not to redevelop before they come out of operation in 2025.[27]
Although the FAO assumes that the Province will redevelop 30,701 long-term care beds by 2028-29, Ministry of Long-Term Care staff informed the FAO that there was no plan or commitment to redevelop any additional long-term care beds, beyond the 15,918 beds announced in the 2021 budget. However, the FAO’s status quo assumption is that the Province will maintain its existing stock of long-term care beds and will redevelop the remaining D class beds with licences that have expired and the B and C class beds with licences that will expire in June 2025. This leads to a minimum long-term care bed redevelopment requirement of 30,701 beds by 2028-29. Note that this plan would still leave an estimated 807 B and C class long-term care beds operated by municipal owned long-term care homes that would not be redeveloped.
Members of the Standing Committee on Estimates may wish to ask the Ministry of Long-Term Care to confirm:
- if all B, C, and D class beds with expired or expiring licences will be redeveloped and under what timelines;
- whether the remaining estimated 807 B and C class beds in municipal-owned homes (which do not have expiring licences) will be redeveloped and under what timelines; and
- what will happen to the B and C class beds with licences that expire in June 2025, if there is no redevelopment agreement by that time.
The following chart outlines the FAO’s assumption that 30,701 long-term care beds will be redeveloped by 2028-29. The FAO projection incorporates actual project timelines for the 15,918 redeveloped beds that have been allocated to date. The projection also assumes that the Province will be successful in either executing development agreements to redevelop the remaining 14,783 beds or reallocating the licences to other LTC operators by June 2025.
Figure 3‑4 FAO estimated cumulative in-service dates for redeveloped beds
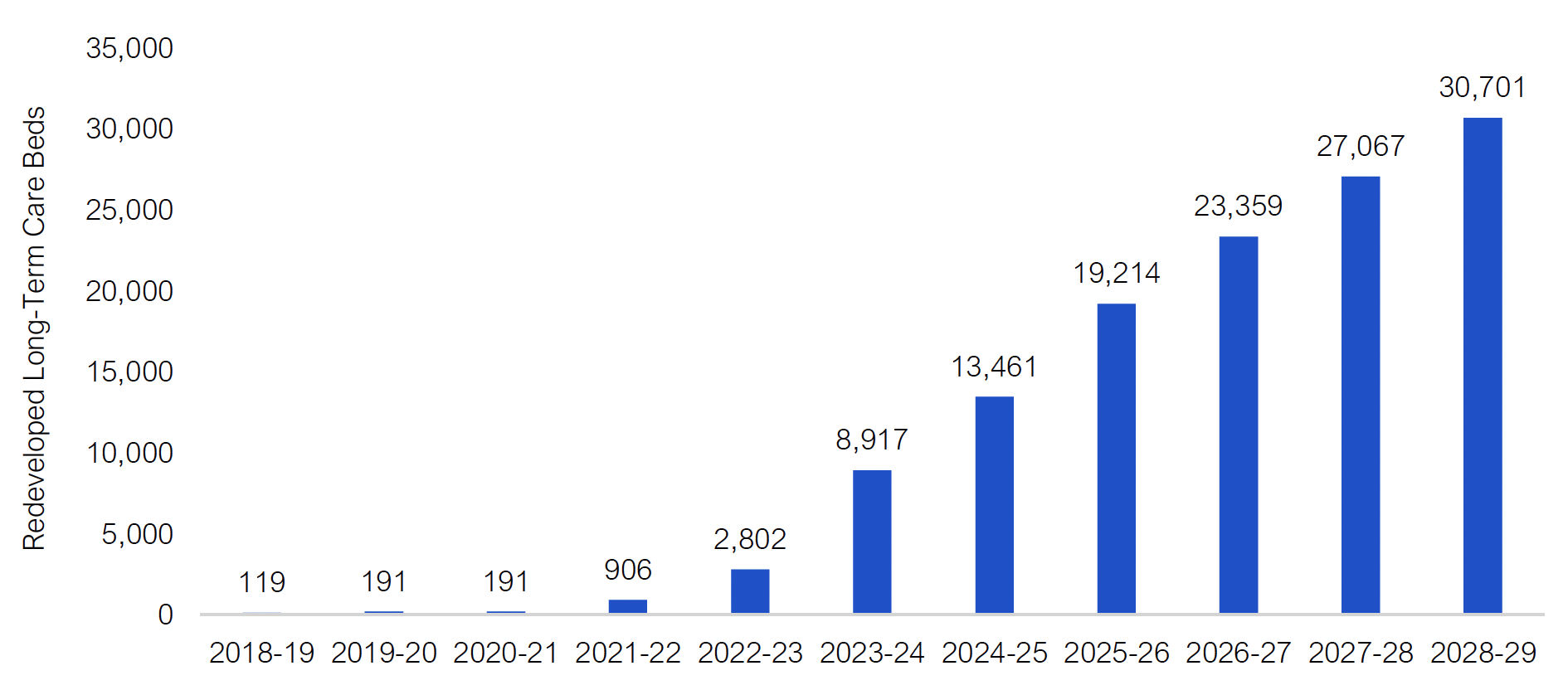
Source: FAO analysis of information provided by MLTC.
Accessible version
| Fiscal Year | Redeveloped Long-Term Care Beds |
|---|---|
| 2018-19 | 119 |
| 2019-20 | 191 |
| 2020-21 | 191 |
| 2021-22 | 906 |
| 2022-23 | 2,802 |
| 2023-24 | 8,917 |
| 2024-25 | 13,461 |
| 2025-26 | 19,214 |
| 2026-27 | 23,359 |
| 2027-28 | 27,067 |
| 2028-29 | 30,701 |
Importantly, the FAO estimates that only 8,917 long-term care beds will be redeveloped by the end of the 2023-24 fiscal year. This is well short of the Province’s 2019 budget commitment to redevelop 15,000 long-term care beds by 2023-24. Overall, the FAO projects that the Province will not reach 15,000 redeveloped beds until 2025-26.
The New Long-Term Care Development Policy
After an LTC home operator signs a development agreement with the ministry to build or redevelop long-term care beds, the LTC home operator is required to finance and construct the beds in accordance with the agreement. Once the LTC home operator has met the requirements outlined in the development agreement, the Province will provide the LTC home operator with a construction subsidy that covers a portion of the construction costs.
Historically, long-term care operators in Ontario have stated that the subsidy provided by the Province did not cover a sufficient portion of the cost of construction. This resulted in limited uptake from the long-term care sector for the Province’s prior efforts to build and redevelop long-term care beds and is part of the reason the Province will not meet its 2019 budget targets of building and redeveloping 15,000 long-term care beds by 2023-24.[28]
In July 2020, the Province introduced a new long-term care development policy to help accelerate the construction and redevelopment of long-term care beds. This new development policy aims to increase uptake by the LTC sector by introducing a new funding model that significantly increases provincial subsidies for new and redeveloped beds. This new funding model provides LTC operators with a daily construction funding subsidy of up to $25.28 per bed per day for 25 years once the bed is in operation, as well as a development grant of up to $51,376 per bed which is paid about three months prior to the bed opening.[29] For comparison, the previous construction funding policy provided a daily construction funding subsidy of up to $23.03 per bed per day for 25 years and no development grant funding.[30]
The FAO estimates that this new policy will increase the maximum construction funding subsidy by 41 per cent from $164,000 ($2021) to $232,000 ($2021) per bed. For perspective, the average cost of construction for a long-term care bed is estimated to range from $346,000 ($2021) to $477,000 ($2021).[31]
This new policy can be applied to all projects with a first resident occupancy date of June 30, 2018 or later, which would cover all 30,000 new committed long-term care beds and most of the assumed 30,701 redeveloped beds.[32] In total, the FAO estimates that this new development policy will increase long-term care spending by over $2.5 billion from 2020-21 to 2029-30.
In addition to the new development policy, the Province also announced a new pilot program to accelerate the construction of new long-term care homes (the Accelerated Build Pilot Program).[33] This program will provide over $600 million in capital funding in 2020-21 and 2021-22 to fast-track the development of four long-term care homes with up to 1,280 beds. The Province is targeting to have these beds in operation by 2022.
LTC Bed Forecast and Risks
Assuming that the Province is successful in creating 30,000 new long-term care beds by 2028-29, and that no existing long-term care beds are taken out of service, the FAO projects that the number of long-term care beds will reach 108,017 by 2028-29.
Figure 3‑5 FAO projection for the total number of funded long-term care beds, 2018-19 to 2029-30
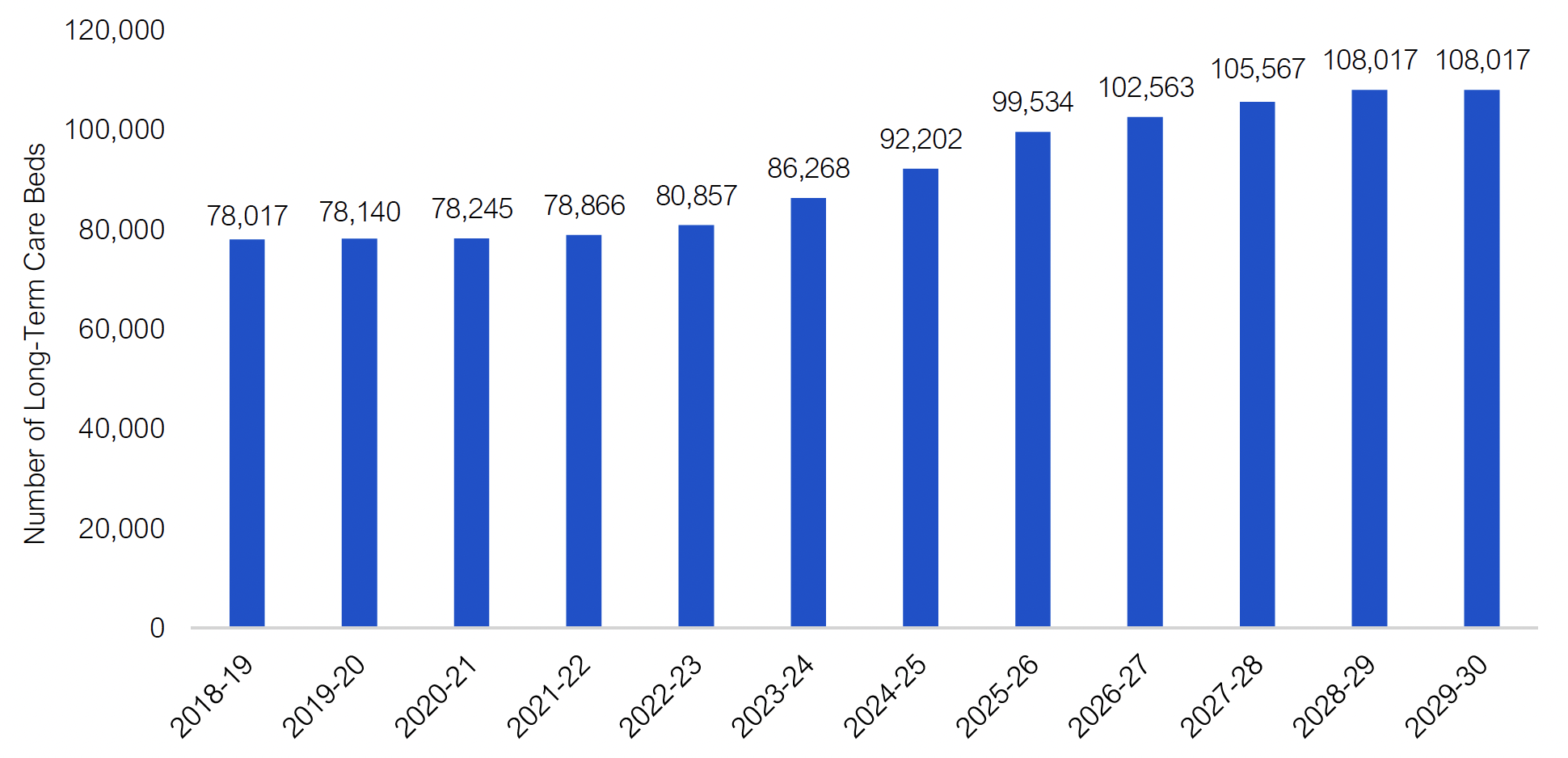
Note: The FAO forecast reflects the number of funded beds, not the number of beds available for LTC residents, as some beds will be under redevelopment or may be unavailable due to infection prevention and control measures
Source: FAO analysis of information provided by MLTC.
Accessible version
| Fiscal Year | Number of Long-Term Care Beds |
|---|---|
| 2018-19 | 78,017 |
| 2019-20 | 78,140 |
| 2020-21 | 78,245 |
| 2021-22 | 78,866 |
| 2022-23 | 80,857 |
| 2023-24 | 86,268 |
| 2024-25 | 92,202 |
| 2025-26 | 99,534 |
| 2026-27 | 102,563 |
| 2027-28 | 105,567 |
| 2028-29 | 108,017 |
| 2029-30 | 108,017 |
However, the FAO has identified three key risks to the FAO’s long-term care bed projection.
Risk: 7,400 Beds May Not Return to Service
As of March 2021, over 7,400 long-term care beds were temporarily not in service due to public health measures to prevent the spread of COVID-19. The ministry has indicated to the FAO that LTC operators must fill vacant beds that are “available” for new and returning residents by September 1, 2021 or they will not be eligible for funding. However, ongoing infection prevention and control measures[34] could mean that many of these beds will continue to be unavailable and some beds may be prevented from reopening entirely. Members of the Standing Committee on Estimates may wish to ask the ministry for more information on how many long-term care beds are expected to be reopened by September 2021 and how many beds are expected to be permanently prevented from reopening.
Risk: Construction Timelines May Not Be Achieved
Previous long-term care bed expansion and redevelopment commitments have not been achieved, which highlights the historic difficulty in meeting long-term care bed expansion and redevelopment targets. For example, in 2014, the Province committed to redevelop 30,000 B, C and D beds by 2025; however, very few beds were redeveloped from 2014 to 2019.[35] Then, in the 2019 budget, the Province committed to add 15,000 new long-term care beds and redevelop 15,000 existing long-term care beds by the end of 2023-24. The FAO estimates that the Province will only build 8,251 new long-term care beds and redevelop only 8,917 beds by the end of 2023-24.
Risk: Long-Term Care Beds with Expiring Licences May Be Permanently Taken Out of Service
As noted above, Ministry of Long-Term Care staff informed the FAO that there was no plan or commitment to redevelop any additional long-term care beds, beyond the 15,918 beds announced in the 2021 budget. This leaves 14,783 long-term care beds with expired licences or licences that are set to expire in June 2025 that do not have redevelopment agreements. The FAO assumes that these beds will be redeveloped to maintain the Province’s existing stock of long-term care beds.[36] Alternatively, the Province could decide to permanently take these beds out of service and reduce its supply of long-term care beds. The ministry recently stated that “further advancement on redeveloping beds will be contingent on future funding availability.”[37] Members of the Standing Committee on Estimates may wish to ask the ministry when it expects that decisions on the availability of redevelopment funding will be made for the remaining 14,783 long-term care beds with expired or expiring licences.
LTC Wait List Considerations
In a 2019 report, the FAO projected that the wait list for long-term care would increase from 34,900 in 2018-19 to 36,900 by 2023-24, even with the assumption that the Province was able to successfully add 15,000 new long-term care beds over this time.[38] Due to uncertainties surrounding the impact of the COVID-19 pandemic, including the current impact of infection prevention and control measures on long-term care bed capacity and any potential impact on the demand for long-term care,[39] the FAO cannot update its wait list projection.
However, to provide context on the potential demand for long-term care beds, over 80 per cent of Ontarians in long-term care are over the age of 75 and growth in this demographic is the key driver of demand for long-term care beds. Between 2009-10 and 2018-19, the Province added only 1,900 LTC beds, which resulted in the number of LTC beds per 1,000 Ontarians aged 75 and over decreasing from 91 in 2009-10 to 73 in 2018-19.
Looking ahead, the FAO projects that the number of Ontarians aged 75 and over will increase by 52 per cent from 2018-19 to 2029-30 while the number of long-term care beds will increase by 38 per cent. As a result, even if the Province is able to increase the supply of long-term care beds by 30,000 by 2028-29, the number of long-term care beds per 1,000 Ontarians aged 75 and over will continue to decrease, from 73 in 2018-19 to 66 in 2029-30. This indicates that the Province’s plan to add 30,000 beds by 2028-29 will likely not be sufficient to keep pace with the growing demand for long-term care from Ontario’s growing and aging population.
Figure 3‑6 Projected number of long-term care beds per 1,000 Ontarians aged 75 and over, 2018-19 to 2029-30
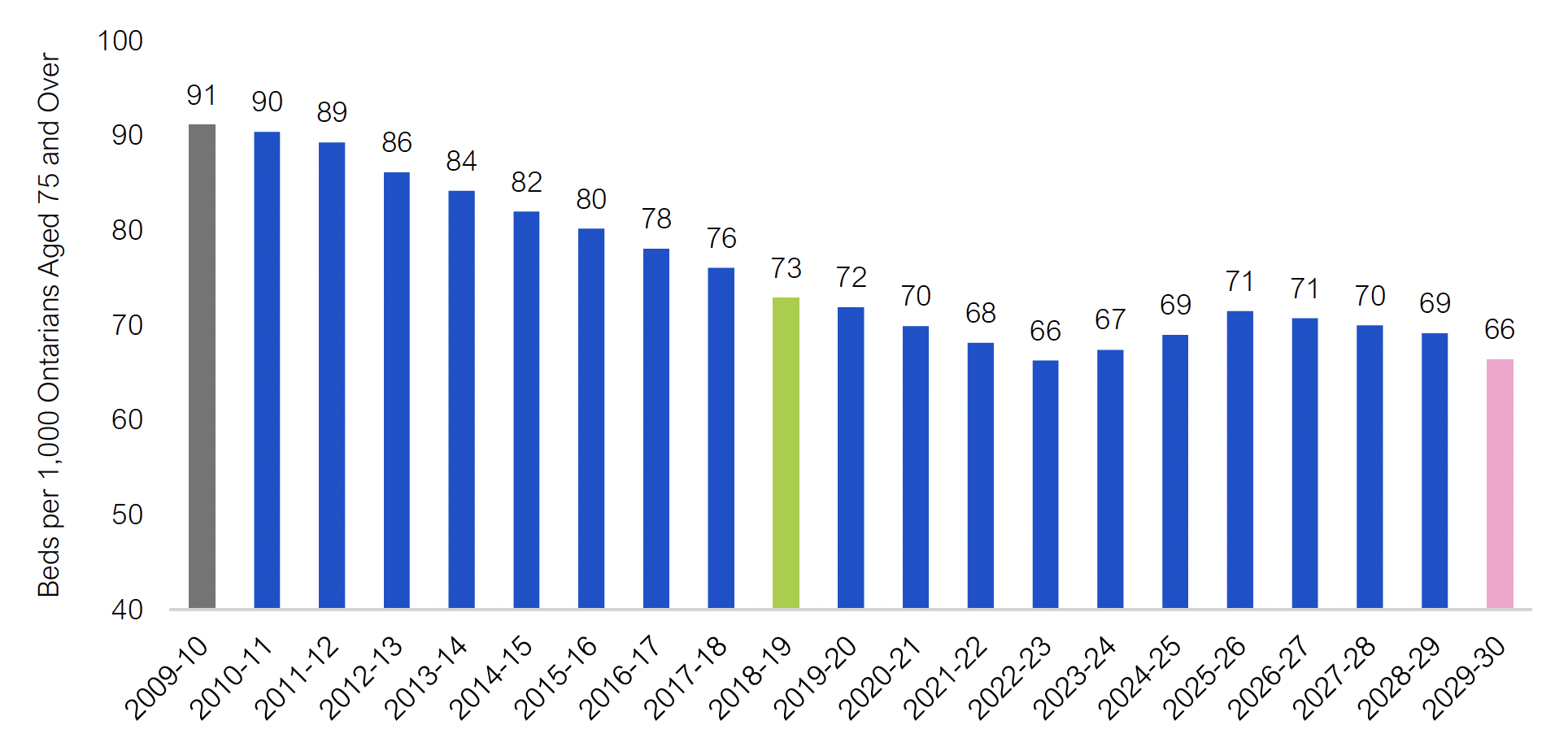
Source: FAO.
Accessible version
| Fiscal Year | Beds per 1,000 Ontarians Aged 75 and Over |
|---|---|
| 2009-10 | 91 |
| 2010-11 | 90 |
| 2011-12 | 89 |
| 2012-13 | 86 |
| 2013-14 | 84 |
| 2014-15 | 82 |
| 2015-16 | 80 |
| 2016-17 | 78 |
| 2017-18 | 76 |
| 2018-19 | 73 |
| 2019-20 | 72 |
| 2020-21 | 70 |
| 2021-22 | 68 |
| 2022-23 | 66 |
| 2023-24 | 67 |
| 2024-25 | 69 |
| 2025-26 | 71 |
| 2026-27 | 71 |
| 2027-28 | 70 |
| 2028-29 | 69 |
| 2029-30 | 66 |
Increasing Direct Care for Long-Term Care Residents
The FAO’s spending projection incorporates the Province’s commitment to increase the average daily direct care hours provided to long-term care residents. This was a recommendation from Ontario’s Long-Term Care COVID-19 Commission and was originally announced in the 2020 Ontario Budget. The Province’s commitment includes:
- Providing long-term care residents with an average of four hours of direct daily care from a nurse or personal support worker.
- Providing long-term care residents with an average of 36 minutes of direct daily care from allied health professionals, including physiotherapists and health care aides.
- Providing funding to recruit and train personal support workers.
In 2018, the Province estimates nurses and personal support workers provided 165 minutes (2.75 hours) and allied health professionals provided 30 minutes of direct care on average per day to residents.[40] The Province’s plan is to increase these amounts to 240 minutes (or four hours) by 2024-25 for direct care provided by nurses and personal support workers and 36 minutes by 2022-23 for direct care provided by allied health professionals.[41]
Figure 3‑7 Targets for increasing average daily direct care hours for long-term care residents
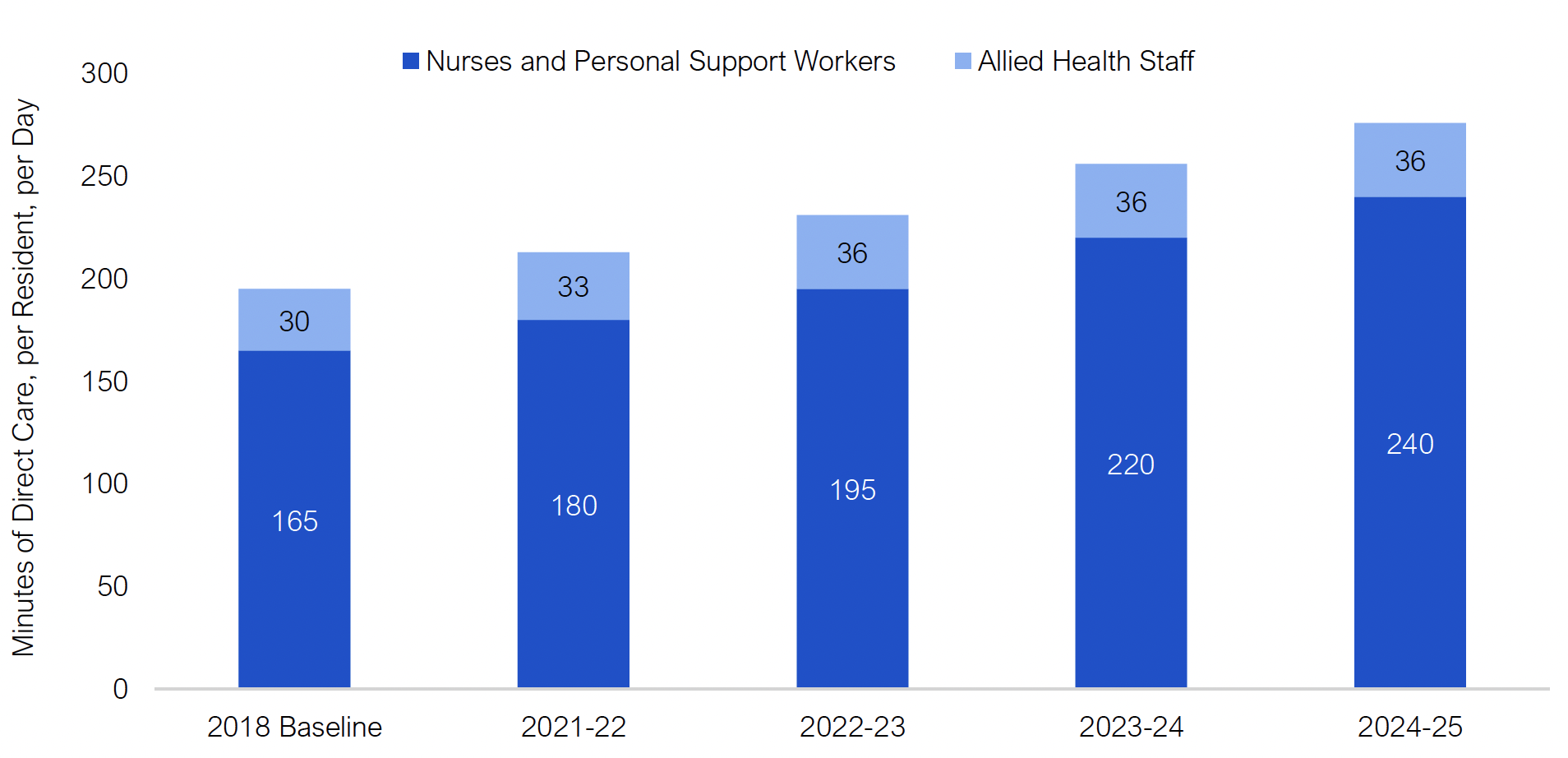
Note: Nurses include registered nurses and registered practical nurses. Allied health staff include activity assistants, health aides, administrators, social workers, physiotherapists and others.
Source: Ontario’s Long-Term Care Staffing Plan (2021-2025).
Accessible version
| Timeline | Minutes of Direct Care, per Resident, per Day | |
|---|---|---|
| Nurses and Personal Support Workers | Allied Health Staff | |
| 2018 Baseline | 165 | 30 |
| 2021-22 | 180 | 33 |
| 2022-23 | 195 | 36 |
| 2023-24 | 220 | 36 |
| 2024-25 | 240 | 36 |
The FAO estimates that these increased care commitments will cost a total of $4.9 billion from 2021-22 to 2024-25. This estimate is similar to the Province’s forecast.
| 2021-22 | 2022-23 | 2023-24 | 2024-25 | Four Year Total | |
|---|---|---|---|---|---|
| FAO Estimate | 546 | 972 | 1,466 | 1,865 | 4,850 |
| Government Estimate | 500 | 1,000 | 1,500 | 1,900 | 4,900 |
| Difference | 46 | -28 | -34 | -35 | -50 |
The FAO estimates that 17,000 personal support workers and 12,200 nurses (registered nurses and registered practical nurses) for a total of 29,200 full-time equivalent positions will need to be hired by 2024-25 to meet the government’s commitment.[42] This is consistent with the Province’s statement in the 2021 budget that the commitment will require hiring more than 27,000 nurses and personal support workers.[43]
Importantly, the 29,200 new full-time equivalent positions by 2024-25 is to support the increase in daily direct care hours and does not include the increase in staff required to support the projected increase in the supply of long-term care beds. In total, the FAO estimates that over 37,000 nurses and personal support workers will need to be hired by 2024-25 to support both the increase in the supply of new long-term care beds and the increase in daily direct care hours. Members of the Standing Committee on Estimates may wish to ask the ministry for further information on its plans to increase employment in long-term care by over 37,000 nurses and personal support workers by 2024-25.
4 | Program Review
This chapter reviews requested and projected spending for the Ministry of Long-Term Care’s 2021-22 Expenditure Estimates by program vote (Supply Bill spending) and other spending (consolidation and other adjustments).[44]
Note: “2020-21 Projected Spending” represents the interim spending forecast for 2020-21 from the 2021 Ontario Budget. The FAO will provide updated 2020-21 spending results in its upcoming Expenditure Monitor report for the fourth quarter of 2020-21.
Vote 4501 – Ministry Administration Program
The Ministry Administration Program supports the delivery of all programs and services offered by MLTC. Vote 4501 includes only one sub-program (item), Ministry Administration, with spending largely for salaries, wages and employee benefits. Vote 4501 does not include any transfer payment programs. The overall spending request is up $1 million, or 15.1 per cent, from 2020-21 projected spending.
| Item | Ministry Administration Program (Vote 4501) |
2020-21 Projected Spending ($ millions) |
2021-22 Estimates ($ millions) |
1 Year Change ($ millions) |
1 Year Growth (%) |
|---|---|---|---|---|---|
| 1 | Ministry Administration | ||||
| Salaries, Wages and Employee Benefits | 4 | 5 | 1 | 21.9 | |
| Services | 1 | 1 | < -1 | -15.9 | |
| Other Spending | < 1 | < 1 | < 1 | 5.7 | |
| Total Supply Vote | 5 | 6 | 1 | 15.1 |
Vote 4502 – Long-Term Care Homes Program
The Long-Term Care Homes Program includes two sub-programs (items): Long-Term Care Homes Program (operating, $6.4 billion) and Long-Term Care Program (capital, $0.5 billion). Three transfer payments account for most of the planned 2021-22 spending in Vote 4502:
- Long-Term Care Homes – Operations at $6.1 billion, which is down $44 million or 0.7 per cent from 2020-21 projected spending.
- Long-Term Care Homes – Development at $0.2 billion. This program had a $103 million budget in the 2020-21 Expenditure Estimates that was not spent, resulting in a year-over-year spending increase of $228 million.
- Long-Term Care Homes Capital at $0.5 billion, which is up $337 million or 179.5 per cent from 2020-21 projected spending.
In addition, salaries, wages and employee benefits is up $16 million, or 51.1 per cent, from 2020-21 projected spending.
| Item | Long-Term Care Homes Program (Vote 4502) |
2020-21 Projected Spending ($ millions) |
2021-22 Estimates ($ millions) |
1 Year Change ($ millions) |
1 Year Growth (%) |
|---|---|---|---|---|---|
| 1 | Long-Term Care Homes Program (Operating) | ||||
| Long-Term Cares Homes – Development | 0 | 228 | 228 | ||
| Long-Term Care Homes – Operations | 6,161 | 6,117 | -44 | -0.7 | |
| Salaries, Wages and Employee Benefits | 32 | 49 | 16 | 51.1 | |
| Services | 9 | 7 | -2 | -23.3 | |
| Other Spending | 2 | 3 | 1 | 48.6 | |
| Total Item | 6,204 | 6,404 | 200 | 3.2 | |
| 2 | Long-Term Care Program (Capital) | ||||
| Long-Term Care Homes Capital | 188 | 525 | 337 | 179.5 | |
| Other Transactions | < 1 | < 1 | 0 | 0.0 | |
| Total Item | 188 | 525 | 337 | 179.5 | |
| Total Supply Vote | 6,392 | 6,928 | 537 | 8.4 |
Other Spending
The financial results of organizations controlled by the Province, including hospitals and certain provincial agencies, are consolidated into the financial results of the Province. In the case of the Ministry of Long-Term Care, a significant portion of the ministry’s spending is recorded as expenses on the financial statements of Ontario Health and with hospitals. Accordingly, negative adjustments are recorded as ‘other spending’ with MLTC and corresponding positive adjustments are recorded as ‘other spending’ with the Ministry of Health.[45]
For 2021-22, the ministry plans to make a $5.6 billion negative ‘other spending’ adjustment to account for planned payments to long-term care home operators that will be recorded as expenses on the financial statements of Ontario Health. This negative adjustment is lower by $1.4 billion compared to 2020-21.
The ministry also plans to make negative ‘other spending’ adjustments to reflect planned payments made by the ministry that will be recorded as spending in the hospitals sector. For 2021-22, there are planned negative adjustments of $48 million for hospitals operating and $525 million for hospitals capital.
| Other Spending | 2020-21 Projected Spending ($ millions) |
2021-22 Estimates ($ millions) |
1 Year Change ($ millions) |
1 Year Growth (%) |
|---|---|---|---|---|
| Operating | ||||
| Ontario Health | -4,163 | -5,574 | -1,411 | -33.9 |
| Hospitals | -109 | -48 | 61 | 56.2 |
| Total Operating | -4,272 | -5,622 | -1,349 | -31.6 |
| Capital | ||||
| Hospitals | -188 | -525 | -337 | -179.5 |
| Total Capital | -188 | -525 | -337 | -179.5 |
| Total Other Spending | -4,460 | -6,146 | -1,686 | -37.8 |
Footnotes
[1] Volume 1 of the 2021-22 Expenditure Estimates is available here: https://www.ontario.ca/page/expenditure-estimates-volume-1-table-contents-2021-22.
[2] If the SCE does not deliver a report to the legislature by the third Thursday in November, then the Estimates are deemed to be passed by the SCE. Standing Orders of the Legislative Assembly of Ontario (SO 66(b)).
[3] Excludes negative adjustments of $4.5 billion in 2020-21 and $6.1 billion in 2021-22 to record expenses on the financial statements of Ontario Health and with the hospitals sector. These negative adjustments are offset by corresponding positive adjustments with the Ministry of Health.
[4] A corresponding positive adjustment is recorded with the Ministry of Health.
[5] Payments for infrastructure assets in the hospitals sector will be expensed over the useful life of the asset.
[6] LTC residents are required to pay accommodation rates (co-payments) for long-term care, which vary based on the type of accommodation they receive (e.g., basic, semi-private or private room). A portion of the payments made by residents for accommodation is remitted back to the Province to offset some of the cost of the long-term care homes program.
[7] For more information on the level of care per diem payments, see Ministry of Health and Long-Term Care, “Policy: LTCH Level-of-Care Per Diem Funding Summary,” August 2019.
[8] Corresponding positive adjustments are included with the Ministry of Health.
[9] Presentation to Ontario’s Long-Term Care COVID-19 Commission, slide 19. http://www.ltccommission-commissionsld.ca/presentations/pdf/Long-Term_Care_Home_Development_Foundational_Redacted_September_21_2020.pdf.
[10] 2021 Ontario Budget, p. 43.
[11] FAO, “Long-Term Care Homes Program: A Review of the Plan to Create 15,000 New Long-Term Care Beds in Ontario,” 2019.
[12] Ontario’s Long-Term Care COVID-19 Commission, Final Report, April 30, 2021, p. 36.
[13] Office of the Auditor General of Ontario, “COVID-19 Preparedness and Management: Special Report on Pandemic Readiness and Response in Long-Term Care,” April 2021, p. 35.
[14] As reported to the FAO by the Ministry of Long-Term Care.
[15] See FAO, “Long-Term Care Homes Program: A Review of the Plan to Create 15,000 New Long-Term Care Beds in Ontario,” 2019, for analysis of the previous LTC bed expansion commitment.
[16] Presentation to Ontario’s Long-Term Care COVID-19 Commission, slide 13. http://www.ltccommission-commissionsld.ca/presentations/pdf/Long-Term_Care_Home_Development_Foundational_Redacted_September_21_2020.pdf.
[17] For the purposes of this report, allocated new or redeveloped long-term care beds refers to beds for which the ministry provided the FAO with information on the location, operator and projected in-service date.
[18] In fact, MLTC estimates that 90 to 95 per cent of redevelopment projects will be new builds as opposed to redeveloping existing spaces.
[19] The D class beds do not meet the standards of the 1972 Nursing Homes Act Regulation but were “upgraded” starting in 2002 by spending an approved amount to benefit resident health, safety or well-being.
[20] Ministry of Health and Long-Term Care, Long-Term Care Home Design Manual 2015.
[21] The remaining 2,971 B and C class beds that do not have expiring licences are operated by municipal owned long-term care homes. Municipal owned long-term care home licences have no specific term.
[22] Ontario’s Long-Term Care COVID-19 Commission, “Government of Ontario, MLTC, Capital Development and Licensing, Transcript, September 18,” 2020, pp. 75-76 and Office of the Auditor General of Ontario, “COVID-19 Preparedness and Management: Special Report on Pandemic Readiness and Response in Long-Term Care,” April 2021, pp. 15 and 21.
[23] The 2,406 beds include a combination of A class beds and municipally owned B and C class beds.
[24] This figure includes 26,531 B and C class beds with expiring licences in June 2025, 1,764 D class beds with expired licences, and 2,406 A, B and C class beds that do not have expiring licences but are already under redevelopment. Given that the licences for the 26,531 B and C class beds expire in June 2025, the FAO assumes that the redevelopments will be complete by 2028-29, or three years after the licences expire.
[25] Long-Term Care Homes Act, 2007, s. 103(1).
[26] Long-Term Care Homes Act, 2007, s. 187(3).
[27] Presentation to Ontario’s Long-Term Care COVID-19 Commission, “Long-Term Care Home Licensing Framework,” slide 14, September 2020.
[28] Ontario Long Term Care Association, Challenges and solutions: Rebuilding long-term care for Ontario’s seniors.
[29] Government of Ontario, Long-Term Care Home Capital Development Funding Policy, 2020.
[30] Ministry of Health and Long-Term Care, Policy: Construction Funding Subsidy Policy for Long-Term Care Homes, 2019.
[31] Robyn Gibbard, Sizing Up the Challenge: Meeting the Demand for Long-Term Care in Canada, The Conference Board of Canada, 2017.
[32] For development agreements signed prior to the implementation of this new policy, the ministry must approve the funding and amend the development agreement.
[33] Government of Ontario, Ontario Unveils New Innovative Approach to Building Long-Term Care Homes Faster, July 21, 2020.
[34] As currently outlined in Directive #3 for Long-Term Care Homes under the Long-Term Care Homes Act, 2007 issued under Section 77.7 of the Health Protection and Promotion Act, R.S.O 1990, c. H.7.
[35] Ontario’s Long-Term Care COVID-19 Commission, “Government of Ontario, MLTC, Long-Term Care Home Development, Transcript, September 21,” 2020, p. 31.
[36] This assumption is reflected in the FAO’s spending projection for the ministry.
[37] Office of the Auditor General of Ontario, “COVID-19 Preparedness and Management: Special Report on Pandemic Readiness and Response in Long-Term Care,” April 2021, p. 37.
[38] FAO, “Long-Term Care Homes Program: A Review of the Plan to Create 15,000 New Long-Term Care Beds in Ontario,” 2019.
[39] In the 2019 wait list forecast, the FAO incorporated a factor that reflected an observed trend of demand for long-term care increasing more slowly than demographics would otherwise indicate. This reflected a declining preference for long-term care in the population. The FAO cannot yet determine the impact of the COVID-19 pandemic on the preference for long-term care and thus cannot update the wait list projection.
[40] Ontario’s Long-Term Care Staffing Plan (2021-2025).
[41] 2021 Ontario Budget, p. 43.
[42] Note that the FAO’s staffing projections reflect the number of full-time equivalent positions (FTEs) that will need to be hired. This may understate the total number of employees that need to be hired as only about 41 per cent of personal support workers, 40 per cent of registered nurses and 39 per cent of registered practical nurses in long-term care homes worked full-time hours in 2018.
[43] 2021 Ontario Budget, p. 27.
[44] Excludes planned standalone legislation (statutory) spending of $314,014.
[45] See, FAO, “Ministry of Health: Spending Plan Review,” 2021.